
Vfrac - Vertebral fracture screening tool
Contact us
If you would like any further information about the study, please contact the study team on Vfrac-study@bristol.ac.uk
Background
Approximately 12% of older adults have an osteoporotic vertebral fracture (meaning broken bone in the back due to osteoporosis). Currently less than one-third of older people with osteoporotic vertebral fractures are diagnosed due to a variety of reasons including delayed presentation because of expectations around back pain by older people, a reluctance to perform spinal radiographs (X-rays) for back pain, and unclear reporting of radiographs. Identifying patients with these fractures is important as it provides the opportunity to intervene with bone protection therapies that can reduce the risk of further fractures by 30-50%.
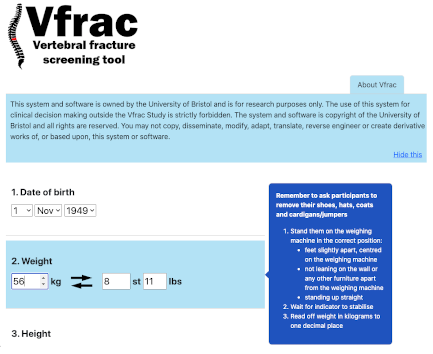
To help address this healthcare gap we have developed the Vfrac decision tool which consists of 15 simple questions based on self-reported data and a physical examination. It takes approximately 5 minutes to perform. The tool can help healthcare professionals decide if an older person presenting to primary care with back pain is at high risk of an osteoporotic vertebral fracture and therefore requires a spinal X-ray.
Earlier work using the Vfrac tool showed that it identified 93% of those with more than one vertebral fracture, and 67% of those with one - considerably better than the one-third currently diagnosed. However, it does need a definitive evaluation to identify it's clinical and cost-effectiveness within primary care.
Before we plan a future definitive trial we need more information to clarify uncertainties including the acceptability of Vfrac to healthcare professionals, and to identify factors that impact on implementation including barriers and facilitators to delivery.
Aim of this study
To optimise use of the Vfrac decision tool within a real-world clinical situation in primary care by
- assessing the acceptability of Vfrac to healthcare professionals (providers) and patients (recipients), and
- identifying factors that impact on its implementation, including barriers and facilitators to delivery.
Findings will be used to develop a series of recommendations to modify Vfrac and improve delivery in the future RCT.
Research plan
We will recruit 6 general practices that vary in terms of size, PCN/cluster and IT system used. By electronic download we will collect anonymised summary data on the number and date of consultations by older women with back pain, resource use after initial consultation for backpain, and new diagnoses since initial consultation for back pain from these six practices.
The Vfrac tool will be implemented in three of the six practices, where primary care staff will be asked to use the tool on female patients over the age of 65 presenting with back pain to determine their risk of having an osteoporotic vertebral fracture. This will help identify which patients should be referred for a diagnostic X-ray.
Two nested studies will also take place within the 3 practices using the Vfrac tool, one will involve a qualitative assessment of acceptability by focus groups/interviews with healthcare professionals and with patients; and the other study will seek to explore the agreement in results to see if Vfrac can be self-completed at home instead of face-to-face.
Research team
The study is co-ordinated from the Musculoskeletal Research Unit within the Bristol Medical School, University of Bristol. The Chief Investigator and clinical lead is Prof. Emma Clark. The Vfrac Research manager is Dr Tanzeela Khalid. Team members include Professor Tim Peters, Dr Lucy Pocock, Dr Zoe Paskins (Keele University), Dr Katie Whale, Dr Eleni Kariki (Manchester Royal Infirmary), Ms Sarah Davis (University of Sheffield), and Dr Sarah Drew.
The VFRAC study is also being supported by Research IT at the University of Bristol and the Musculoskeletal Research Unit's patient involvement group: PEP-R.
Funding
This study is funded by the Research for Patient Benefit Scheme, National Institute for Health Research (reference number NIHR203026).